Scientists at the Paul Scherrer Institute PSI’s Centre for Life Sciences have shown for the first time how genetic defects profoundly alter the internal architecture of human cilia. The results of their study indicate that the structural damage varies depending on the mutation – possibly indicating the existence of previously overlooked subtypes of a poorly understood disease: primary ciliary dyskinesia (PCD). The study was published in the journal Frontiers in Molecular Biosciences.
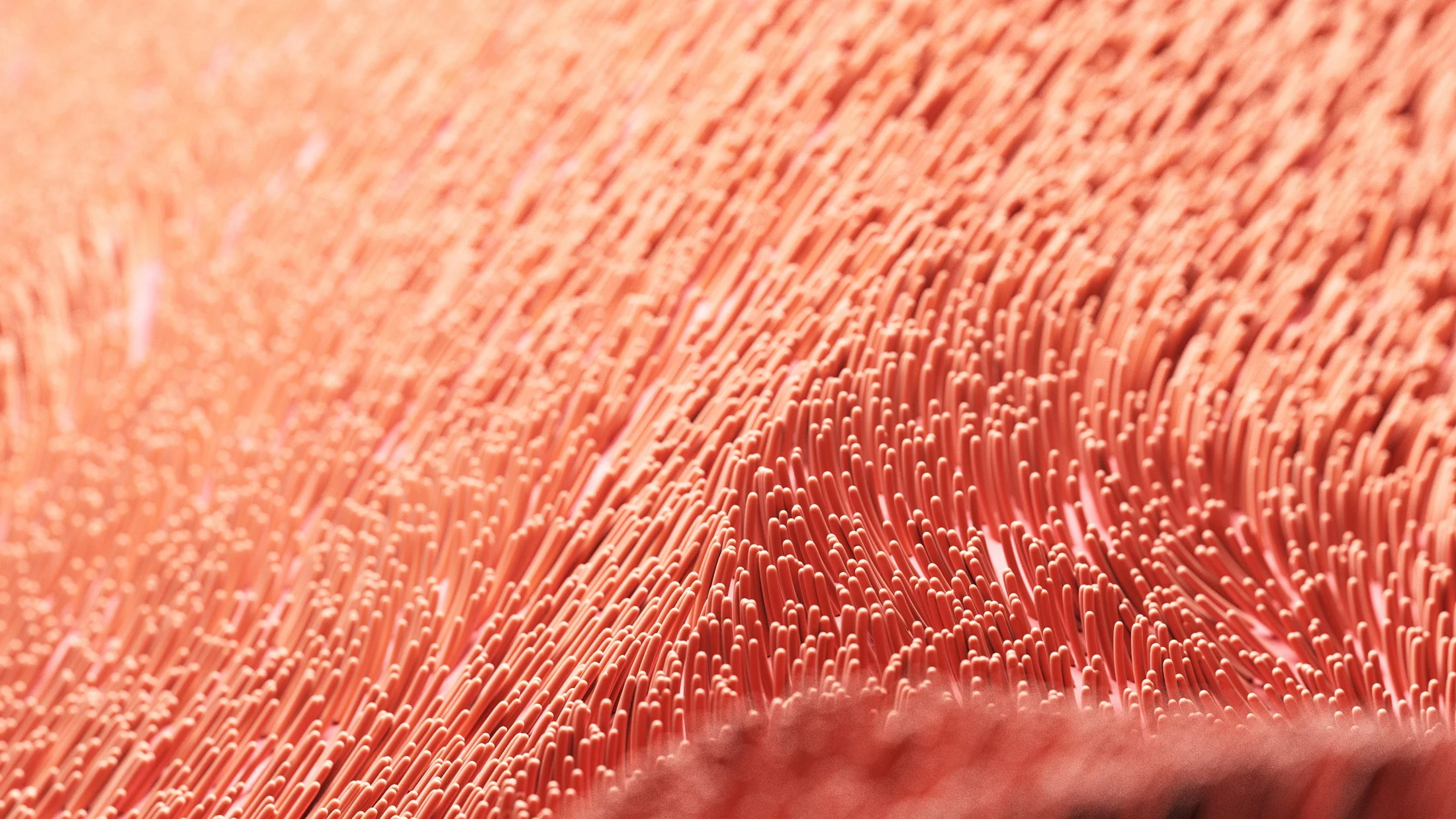
Cilia are tiny, hairlike projections that are capable of movement and are found on the surface of certain cells in our bodies. These membrane protrusions perform vital functions and serve, among other things, to move around entire cells or to transport mucus and fluids. If they fail or don’t move as they should, the consequences can be very serious: chronic respiratory infections, infertility, mirror-image reversal of the internal organs, and complex heart defects.
Although these symptoms appear very different on the surface, they are all manifestations of primary ciliary dyskinesia (PCD), a rare genetic disorder that affects ciliary motility. This condition, which occurs in approximately one in 7,500 to 10,000 cases, is caused by a defect in the structure and function of the cilia. The underlying genetic mutations – often located on the gene DNAH5 – manifest themselves in characteristic but highly variable symptoms. PSI researchers have now succeeded in uncovering the molecular basis of these.
Primary ciliary dyskinesia (PCD) is a rare genetic disorder in which cilia – motile structures found on the surface of many cells – do not function properly. It probably affects around 1 in 7,500 to 10,000 people.
Cilia play an active role in the respiratory tract, middle ear, fallopian tubes and sperm and are used for transport. In PCD, they may not function at all or else their movements may be uncoordinated. This can lead to chronic coughing, recurrent upper respiratory tract infections, middle ear infections with hearing loss, and infertility. Around half of those affected also exhibit situs inversus, whereby their internal organs are arranged in a mirror-image configuration. If left untreated, PCD can lead to severe lung damage. This makes early diagnosis crucial.
A new study by a team led by PhD student and first author Charlotte de Ceuninck together with Takashi Ishikawa from the Laboratory for Multiscale Bioimaging at PSI’s Center for Life Sciences reveals that not all DNAH5 mutations have the same effect. Depending on the precise location of the mutation within the gene, not only the motility of the cilia is affected, but their entire internal architecture changes. Molecular differences that have so far remained hidden using conventional diagnostic methods are now coming to light. “At the molecular level, the research marks a breakthrough,” say de Ceuninck and Ishikawa. The study was published in the journal Frontiers in Molecular Biosciences.
Anatomy of a cilium
Cilia have a highly organised internal framework known as the axoneme. It consists of nine sets of doublet microtubules – tubular protein structures – which are arranged in a ring around two central single tubules. This typical “9+2” structure provides the mechanical basis for the movement of the cilia.
Molecular “motors” are arranged along this scaffolding: dynein arms that convert chemical energy into rhythmic movements. The protein DNAH5 is a key component of the outer dynein arm. Without it, the cilia cannot move – one of the key features of PCD.
Until now, researchers believed that all DNAH5 mutations led uniformly to a loss of the outer dynein arm. However, this latest study reveals a much more nuanced picture. The type of mutation not only determines whether the dynein arm is missing, it also affects the extent to which the entire ciliary structure is disrupted.
Three patients – one picture? Not quite
In their study, the scientists analysed cell samples from three people with PCD who had different DNAH5 mutations. Initial classical diagnostics – including high-speed video microscopy, immunofluorescence and transmission electron microscopy – revealed a consistent pattern: the cilia were immobile, the outer dynein arm was missing.
However, advanced methods produced a more nuanced picture. Using mass spectrometry, the scientists ascertained the protein composition of the isolated cilia. On top of this, they carried out a high-resolution, three-dimensional reconstruction of their internal structure using cryo-electron tomography. The scientists found that the internal composition of the cilia differed significantly depending on the type and position of the mutation in the DNAH5 gene.
This finding is at variance with the previous notion that all mutations in this gene have a similar structural effect. Instead, it is clear that the diagnosis of “PCD” encompasses very different molecular forms of the disease.
Structural loss beyond what was expected
This study focused on the outer dynein arms. However, in some patients the inner dynein arms (IDAs) are affected – along with the nexin-dynein regulatory complex (N-DRC), a key linking element that coordinates the movement of the cilia.
In some cases, parts of the intracellular transport system, the IFT complex, which is responsible for the maintenance of the cilia, can be reduced. Notably, mutations that cause premature termination of translation, known as truncating mutations, typically lead to a more extensive loss of axonemal proteins than mutations in which translation terminates later.
From this it follows that the position of the mutation within the gene affects which ciliary structures become dysfunctional, despite the clinical symptoms of the people affected appearing almost identical. This highlights the importance of molecular analyses for the differentiated diagnosis of rare diseases such as PCD.
Unexpected discoveries: New building blocks of the cilium
In addition to the anticipated loss of proteins, the scientists also identified three proteins that were not previously known to be components of human cilia: CFAP97, VWA3B and DTHD1. These proteins were found in healthy cilia. However, they were completely absent from samples taken from patients with a DNAH5 mutation.
The unknown role of these proteins in the structure of cilia and for motility control opens up new perspectives for both fundamental research and clinical applications, such as future diagnostic procedures, or treatments that could replace the missing proteins using mRNA techniques.
Conclusion: A more complex picture of PCD
The results suggest that primary ciliary dyskinesia should not be viewed as a uniform condition. “The molecular diversity we have observed could explain why the clinical course and the symptoms of the disease vary so greatly,” says Charlotte de Ceuninck.
In future, identifying such subtypes – for example, through high-resolution proteomic analyses to comprehensively examine the protein composition of cells – alongside cryo-electron tomography could pave the way for early diagnosis. This, in turn, would allow therapeutic interventions to begin earlier, helping to halt or slow the progression of lung damage, hearing loss or fertility disorders. “Once we have a better understanding of the molecular differences, we will not only be able to recognise the disease sooner, but also apply more targeted treatments,” adds Takashi Ishikawa.
Contact
Original publication
Proteomic and structural comparison between cilia from primary ciliary dyskinesia patients with a DNAH5 defect
Charlotte de Ceuninck van Capelle, Leo Luo, Alexander Leitner, Stefan A. Tschanz, Philipp Latzin, Sebastian Ott, Tobias Herren, Loretta Müller, Takashi Ishikawa
Frontiers in Molecular Biosciences, 17.07.2025
DOI: 10.3389/fmolb.2025.1593810