Proton therapy has revolutionised mankind’s battle against cancer and saves the lives of numerous children and adults with difficult-to-treat tumours. However, the worldwide rise of this treatment method might never have happened without the pioneering work at the Paul Scherrer Institute PSI. A recently published book tells the story of scientists and physicians at PSI developing this life-saving technique.
Several decades ago, researchers at PSI turned their understanding of basic science into medical application, developing a technique that can cure cancer. The idea was to deliver protons − positively charged particles − to tumours, thus destroying the malignant cells. This therapy – as we now know − is very effective, but demands precision and leaves little room for errors.
The recently published book “Physics against Cancer” by Damien Weber and Simon Crompton delves into the history of proton therapy at PSI, catching the spirit of a group of researchers persevering to make their ideas a reality.
Eradicating tumours
In proton therapy, a concentrated proton beam kills cancer cells by destroying their DNA. Conventional radiation therapy works on the same principle, but uses X-rays rather than protons.
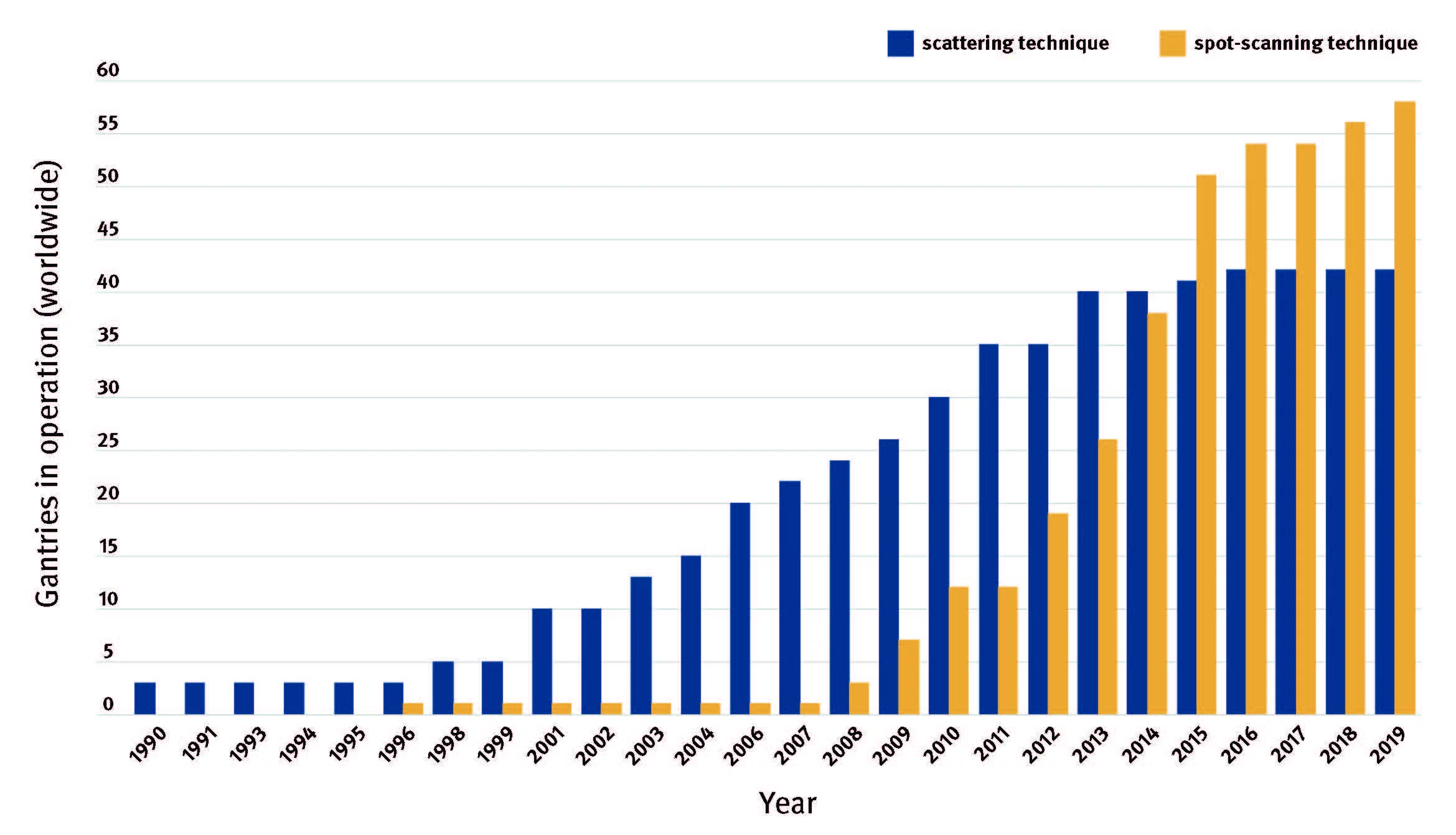
The technique that made proton therapy a worldwide success is pencil beam scanning, also called spot scanning, developed at PSI. A deep-seated tumour is scanned point by point with the pencil-thin proton beam - as if it were being filled in with pencil dots - dot by dot and row by row in three dimensions.
The medical world was initially sceptical as the technology seemed too unmanageable at the time. Researchers at PSI, though, were firmly convinced they could master the technology. “We considered ourselves pioneers in advocating proton therapy for the treatment of cancer and making it work,” says Damien Weber, senior clinician and head of the Center for Proton Therapy at PSI. Meanwhile, pencil beam scanning has become a standard procedure worldwide and since 1996 has been used to treat over 2000 cancer patients at PSI alone.
How it all began
Initially, PSI researchers focused on another, quite exotic particle to treat cancer patients: pions, a type of subatomic particle produced when accelerated protons hit matter. Negatively charged pions had been found to have a promising therapeutic potential when delivered to a tumour, so first radiobiological experiments on pions began at the Swiss Institute for Nuclear research (which was later to become PSI) in the 1970s. In a machine called a piotron, built at PSI, pions were generated and then focused on patients.
In the 1980s, the researchers’ interest shifted to protons, which were lighter, easier to deliver and showed less toxicity. “It seemed the ideal particle,” says Weber. The work with pions wasn’t lost, though: “The legacy of the piotron program was pencil beam scanning. It was because of our experiences with spot scanning in the piotron that we implemented the technique in proton therapy.”
It was no coincidence that proton therapy was developed at a research institute like PSI, as the technology behind it is in fact applied accelerator physics. To control the beam and the magnets, one needs measurement devices, ultrafast electronics and above all, highly qualified people with the skills to build such a machine. These can’t be found in hospitals.
First patients
A clinical highlight at PSI was celebrated in 1984 when the first ever patient in Europe was treated with protons. He was suffering from a rare eye tumour, a uveal melanoma. This was an important first step in the history of clinical application as eye tumours are easy to reach from the outside via irradiation and relatively small in volume. Here, pencil beam scanning is not needed.
Indeed, the first patient ever treated using pencil beam scanning was not even human. She was a dog called Jessie. That was in 1994, a time when no one else in the world was delivering radiation with spot scanning. “We were actually scared to use the technology on patients,” Damien Weber admits. “All we had were calculations and simulations, but we didn’t know what would actually happen in the real world in a patient.”
In 1993, a collaboration with the university vet clinic in Zürich had begun, and PSI treated pets suffering from cancer – mostly cats and dogs. This first patient, Jessie, was a four-year-old Airedale terrier with a huge infiltrative lipoma (a tumour arising in fatty tissue) on her hind leg. Jessie survived well with her tumour stabilized. The response in the pets was just as foreseen by our simulations, so it gave us the green light to go and treat our first human patient with pencil beam scanning,” Weber says. This happened in November 1996: a world premiere.
PSI developed yet another technique that made proton therapy a success: intensity modulated proton therapy, or IMPT. It enables the correct dose of protons to be more accurately targeted to every part of a tumour.
Always improving proton therapy to give better treatment
By 2021, around 250,000 people had been treated with proton therapy globally. Nearly all new centres use pencil beam scanning and modulation techniques based on PSI’s pioneering work.
But the story doesn’t end here: researchers at the Center of Proton Therapy at PSI are still improving proton therapy for the sake of the patients.
Among others, they are testing the FLASH technique that can deliver ultrafast, high-dose irradiation with protons, possibly saving patients many weeks of treatment. Clinical trials into treating tumours in organs that move with the breath such as the lung is another advancement. Moreover, PSI is taking a closer look at the novel approach of proton minibeam radiotherapy in which irradiation through submillimetre-large beamlets takes place on only very small areas of the tumour. Researchers hope it might make it possible to increase the dose, which is needed to fight cancer cells, without increasing the side effects on a patient.
Text: Brigitte Osterath
© PSI provides image and/or video material free of charge for media coverage of the content of the above text. Use of this material for other purposes is not permitted. This also includes the transfer of the image and video material into databases as well as sale by third parties.
Contact
Prof. Dr. med. Damien Charles Weber
Head and Chairman of the Center for Proton Therapy
Paul Scherrer Institute PSI
+41 56 310 58 28
damien.weber@psi.ch
Original Publication / Book
Damien Weber and Simon Crompton: “Physics against Cancer – How the Paul Scherrer Institute pioneered modern proton therapy”, vdf Hochschulverlag at ETH Zurich, 2023.