This page is devoted to a step-by-step explanation of how PSI uses proton therapy to treat deep-seated tumours in order for you to better understand the procedure, and specific details of your therapy and help you find your way around the Center for Proton Therapy.
Request or referral
Most of our patients are referred to us by radiation oncology departments of university clinics and hospitals at home and abroad.
If the tumour with which you have been diagnosed is one of those listed in the indication list published by the Federal Office of Public Health (Bundesamt für Gesundheit – BAG) you, yourself, are entitled to approach us. Contact with your own doctors is of paramount importance since it guarantees that you will be taken good care of before proton therapy begins and after it has been completed.
The tumour board
The decision to administer proton therapy to you or your child at PSI is taken by an interdisciplinary team of doctors and medical physicists that constitute a so-called tumour board. The tumour board meets once a week. In addition to our in house specialists, most tumour boards also involve physicians from other hospitals who participate in tumour board consultations via video conference.
The specialists review your medical history taking into consideration all relevant scans and reports, and results from previous examinations and treatments. Following joint discussions, the board decides whether proton therapy is suitable for you or your child and how best to administer it. If the board decides that proton therapy is not suitable for you or your child, the doctors recommend an alternative form of treatment.
First consultation with the doctor
Our patient office will invite you to a first consultation with one of our radiation oncologists, where you will be informed in greater detail about the therapy, treatment objectives and possible side effects. Within the framework of this consultation you will also be informed (where applicable) of the possibility of taking part in appropriate studies. You can decide at your leisure whether or not you wish to participate. A physical exam is also part of this first consultation, providing the doctor with a comprehensive picture of you and your illness, or that of your child. You are welcome to ask any questions you may have regarding treatment during this consultation.
Preparatory examinations
In general, two medical imaging examinations are necessary in order to plan radiation treatment: a Magnetic Resonance Imaging (MRI) and a CT (computed tomography) scan, the so-called planning CT. The images are superimposed over one another, giving an accurate picture of the location and extent of the tumour, and allowing the therapy planning team to begin drawing up treatment procedures.
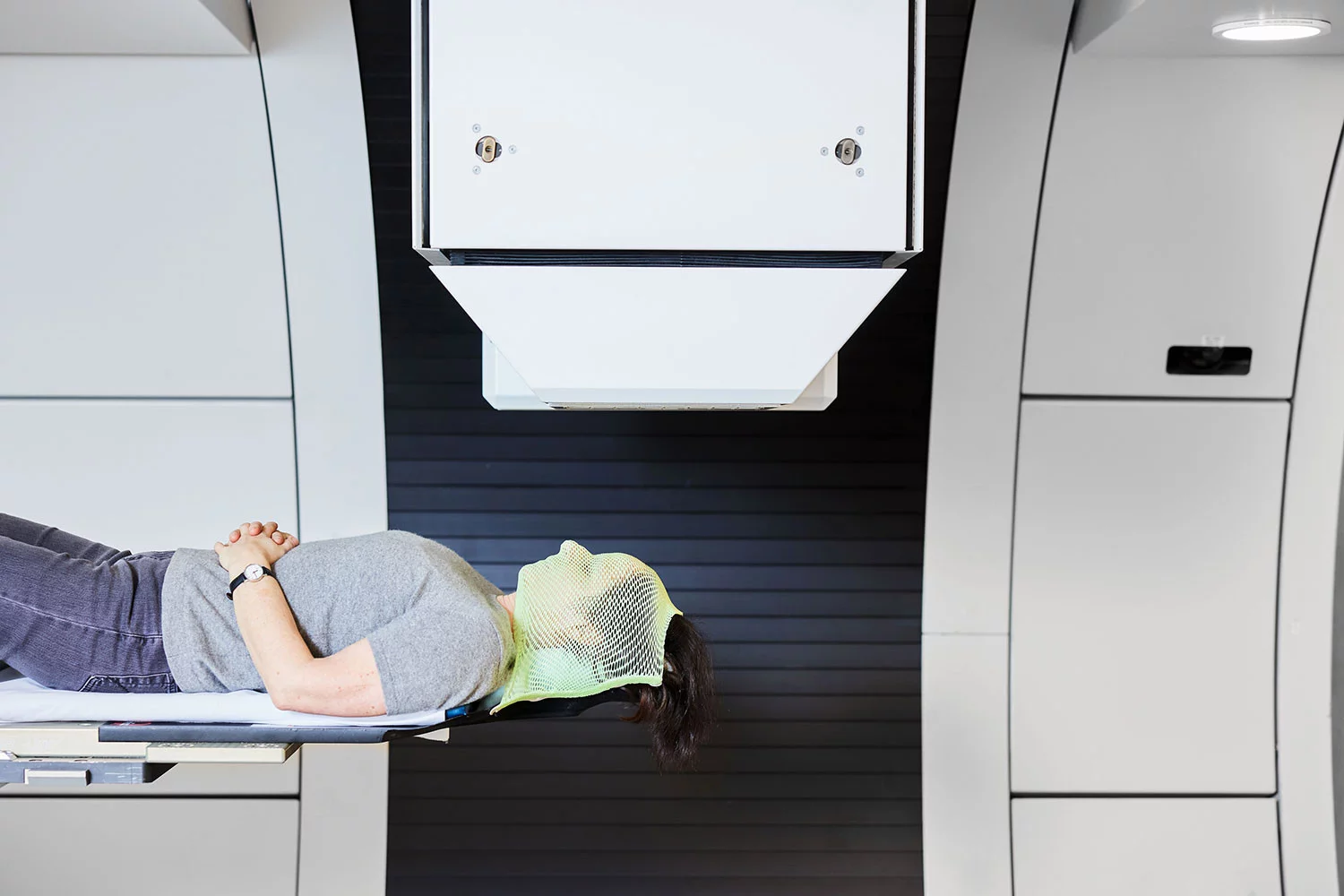
Important and highly individual: positioning
Immediately before or after the medical imaging examination, the radiation therapists (RTTs) construct the patient’s individual positioning cushion. This is a cushion made either for the whole body or for the body area to be irradiated.
The cushion is intended to help you or your child maintain the same position during each radiation session. This is a very important factor in precision- based proton therapy. It also ensures that you, as the patient, are as comfortable and relaxed as possible for the entire duration of the radiation treatment.
We use two kinds of positioning cushions: vacuum cushions or those made with the material used for especially fine-grained contour mattresses (resin-coated Styrofoam pellets). If an area of the head is to be irradiated, you will be given a fitted face mask or a specially made device fitted with your dental impression onto which you can bite during treatment.
Treatment planning
Treatment planning is based on the planning CT and MRT results. Radiation oncologists draw up a treatment plan in cooperation with medical physicists using computer programmes developed at PSI.
Therapy planning contains information both on the precise arrangement of the designated treatment equipment for you or your child, and on proton beam intensity and direction.
Our objective is to optimise proton therapy so that the dose reaching the tumour is high enough to destroy the tumour, while inducing minimal side effects on the tissues immediately surrounding the tumour. To achieve this result, the planning team calculates the optimum beam projection as well as proper dosage, setting the required radiation dose for every spot of the tumour target volume. In order to ensure that all tumour cells are reached, a safety margin around the tumour itself forms part of this calculation. The planning process also takes into account and limits the level of (undesired) normal tissue irradiation around the tumour.
Regular radiation sessions
Once the treatment plan has been drawn up, you will be asked to start your course of radiation. From this point onwards, you’ll be coming to PSI four or five times per week over a period of one-and-a-half to two months. If you need to attend other important appointments during this time, please inform the secretaries early on so that we can make an effort to accommodate these obligations when planning your radiation sessions.
You should calculate about one hour for each radiation session—including preparation and minimal waiting time. At the start of each radiation session, the team will carry out precise controls to ensure your correct positioning on the treatment machine, or that of your child. This is essential to ensure that the beam targets the tumour with optimum accuracy. For this purpose, two X-rays are taken using a small dose of radiation. The radiation therapist (RTT) then compares these with the planning CT: if your current body position differs from that on the planning CT scan, either you or the treatment couch will be re-positioned until you are correctly aligned.
You will not feel anything during the irradiation itself. If you are being irradiated from different directions, you’ll notice that the radiation device and possibly also your treatment couch is moving to find its new position. Depending on the size of the tumour being irradiated, each radiation session takes between 1–45 minutes. During this time, you or your child are alone in the room, but will receive a microphone so that RTTs in the adjoining room can constantly monitor the radiation session via intercom and cameras.
During irradiation you can listen to music. Some patients sleep during treatment. A weekly consultation with your radiation oncologist is part of the planned schedule.