“Fewer side effects with cancer irradiation using protons”
Targeted destruction of tumours with fewer side effects? MD Barbara Bachtiary explains how this is possible with high-precision proton irradiation, using the example of head and neck cancers.
Dr Bachtiary, what is the particular initial situation for cancer in the head and neck area that requires irradiation?
In the event of cancer in the head and neck area, tumours are in the vicinity of sensitive structures like the salivary glands, structures in the oral cavity, mucous membranes in the throat, the larynx, the spinal cord and the brain tissue. During treatment, it is important to protect this healthy tissue in order to reduce side effects and improve the patients’ quality of life.
What does this mean for irradiating tumours in such a sensitive area?
Irradiating the oral cavity and mucous membranes in the throat can result in permanent damage to the swallowing muscles, which means that the patient can no longer take in adequate amounts of nutrients by eating normally and sometimes even needs a feeding tube. Irradiating the parotid glands can cause very unpleasant dryness of the mouth that also impedes food intake as well as speech.
With the proton therapy that PSI has used for over 30 years to treat cancer patients, sensitive organs at risk can be better protected. Why is this?
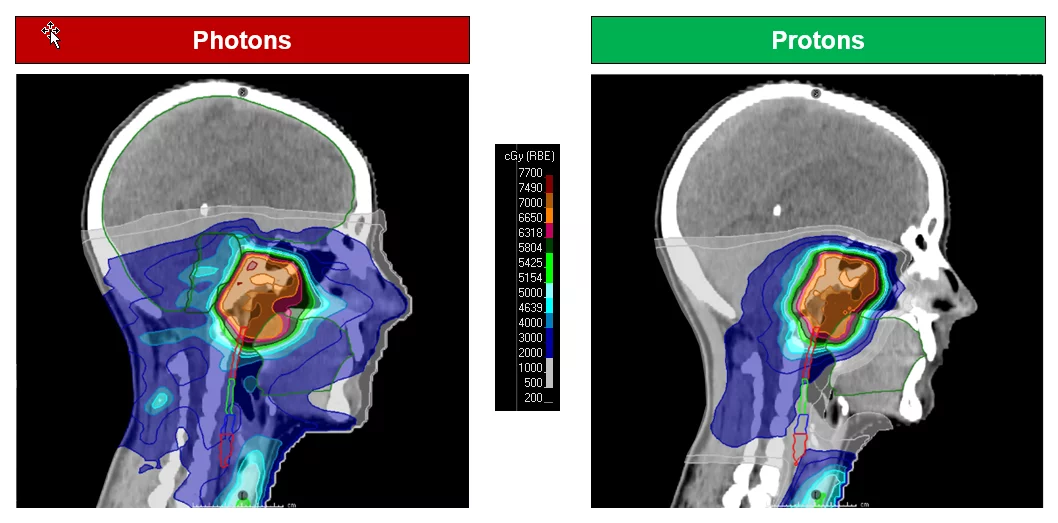
The advantages of proton therapy compared to the usual irradiation with photons, that is X-rays, can be traced back to the unique physical characteristics of protons. In fact, the major part of proton radiation is only emitted in a very narrow range at depth, right where the tumour is, and practically no radiation escapes the tumour to affect healthy tissue in its vicinity. On the one hand, because of this so-called “Bragg peak” at the end of the proton beam’s range a higher dose for improved destruction of the tumour can be administered. On the other hand, a reduction of radiation exposure in the normal tissue and thus a reduction in side effects can be achieved.
Are there clinical studies that substantiate proton therapy’s advantages when used against head and neck tumours?
Yes, these clinical studies show that proton therapy can have advantages in comparison to photon radiation. This applies particularly to unilateral tumours of the head and throat and to advanced tumours in the nasopharyngeal area or sinuses. In the event of re-irradiation, proton therapy can also be beneficial.
How do you decide whether a patient should be considered for proton therapy?
The extent to which healthy tissue can be protected compared to treatment with photons differs from patient to patient. This is why we prepare comparative treatment plans in order to assess whether proton therapy has advantages over photon therapy for individual patients.
As you have already mentioned, irradiation with protons is more protective. Why is it that this form of treatment is still less widespread?
The total potential of proton therapy is not yet sufficiently known in all professional circles. Also, there is only a single proton centre in Switzerland. Depending on the patient’s place of residence, a daily commute to the centre can be long and strenuous. That’s why some patients rent a room near the proton centre for the duration of their treatment. Unfortunately, the travel and accommodation costs are not covered by health insurance. For several patients, these costs, which they must bear themselves, certainly represent a barrier. However, our patient office supports the patients as far as possible.
What other kinds of tumours are irradiated using this technology at PSI?
At PSI, we also treat specific brain tumours, tumours close to the spinal cord and sarcomas. All children that need targeted radiotherapy are also treated using proton therapy.
As someone interested in the treatment or as the parent of a child with cancer, how can I get in touch with you?
If patients need radiotherapy and want to know whether proton therapy would be beneficial, they should talk to their radio-oncologist directly. The oncologist will then contact PSI and discuss the case with PSI physicians at a Tumour Board Meeting. Generally, patients can also contact us directly with their enquiries.
Interview with
MD Barbara Bachtiary
Senior radiation oncologist
Center for Proton Therapy
Paul Scherrer Institute PSI, Villigen AG
Specialist literature
Past, present and future of proton therapy for head and neck cancer
Xingzhe Li, Anna Lee, Marc A Cohen, Eric J Sherman, Nancy Y Lee,
DOI: 10.1016/j.oraloncology.2020.104879