Bench-to-bedside successes: Fruitful collaborations at PSI’s Center for Radiopharmaceutical Sciences make bringing Terbium-161 to the clinic a reality.
Terbium-161 is one of several novel radioisotopes under development at PSI’s Center for Radiopharmaceutical Sciences (CRS) to treat cancer. When linked to a ligand that binds to a target found specifically (or overexpressed) in cancerous cells, the radioisotope enables highly targeted radiotherapy. Terbium-161, which is subject to beta decay, is particularly exciting for therapeutic reasons because it produces abundant short-range ‘Auger’ electrons. This means that the peak of the radiation dose is delivered within the cell. Consequently, terbium-161 is more effective at achieving targeted destruction of cancer cells than, for example, lutetium-177, a more established therapeutic beta-emitting radionuclide.
Now, almost 10 years and over 20 publications into the PSI terbium story, and a long-standing collaboration between the groups of Cristina Müller (Nuclide Chemistry, CRS) and Nick van der Meulen (Radionuclide Development, CRS/LRC) has made exciting advances that bring clinical application of terbium-161 onto the horizon. In particular, a prize and two recent publications have taken important steps to bridge the gap between bench and bedside, culminating in an SNSF project with University Hospital Basel, planned for 2022.
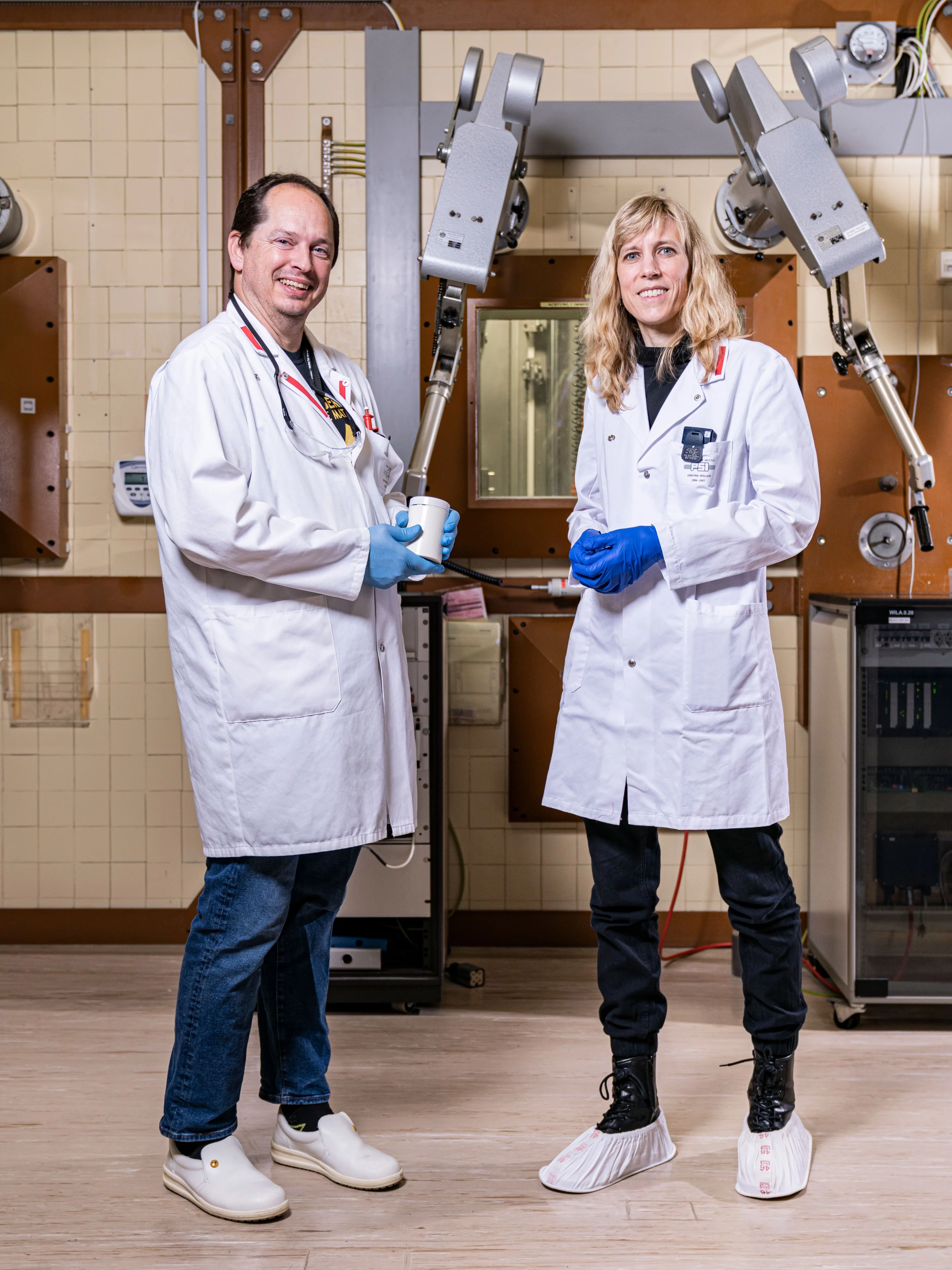
Key to the success of terbium-161 is the unique set-up at PSI, which incorporates on one campus the different steps of preparing radionuclides – a complex procedure, performed in lead shielded cells - and developing them for pharmaceutical use.
“Terbium radionuclides are purified on-site at PSI by Nick van der Meulen and his team, and my team then use and investigate them for therapy and imaging,” explains Cristina Müller. “We pass each other in the corridor almost every day, and can easily bounce ideas off each other and troubleshoot if something is not working. It’s a rare opportunity to have these research activities together in one laboratory.”
Attracting clinical attention: European Journal of Nuclear Medicine and Molecular Imaging (EJNMMI) 2020 Best Paper prize
In a recent success, Müller, van der Meulen and colleagues won the European Journal of Nuclear Medicine and Molecular Imaging (EJNMMI) 2020 Best Paper prize for their publication, ‘Terbium-161 for PSMA-targeted radionuclide therapy of prostate cancer’. In it, they describe a preclinical use of terbium-161 to treat prostate cancer, and highlight to clinicians the clear advantages of terbium-161.
Müller’s group linked terbium-161 to ligands targeting prostate-specific membrane antigen (PSMA), a glycoprotein found on the surface cells in all prostrate tissue, but overexpressed in prostate cancer cells. They then tested terbium-161 conjugates in-vitro and in tumour-bearing mice, and compared them to equivalent lutetium-177 conjugates, demonstrating the dramatically superior therapeutic effect of terbium-161.
Part of the challenge of moving terbium-161, or any new radionuclide, from bench to bedside, is in attracting the attention of clinicians. By strategically publishing their successful preclinical results in a clinical journal, European Journal of Nuclear Medicine and Molecular Imaging, and by using the already clinically-employed PSMA ligand, they were able to draw attention to the benefits of terbium-161 from clinicians.
“PSMA has evolved as one of the most successful targets for nuclear oncology purposes - Novartis are currently in phase III clinical trials with lutetium-177 linked to PSMA-617. Therefore, clinicians are already familiar with this ligand and are interested to consider terbium-161 as an alternative to lutetium-177,” explains Cristina Müller.
Studying the subcellular localisation
An important question, crucial for optimising the terbium-161 therapeutic effect, is where exactly in the cell the radiation dose is delivered. Achieving the maximum therapeutic benefit from the short-range electrons is dependent on the type of ligand that terbium-161 is bound to and the subcellular location of its receptors. In another successful preclinical study, published recently in the European Journal of Nuclear Medicine and Molecular Imaging, Müller’s team investigated the effect of subcellular localisation of terbium-161 labelled antagonists to optimise treatment of neuroendocrine neoplasms – tumours that arise from cells of the endocrine and nervous systems. They investigated ligands that brought terbium-161 to different areas of the cell; namely the cell cytoplasm, the cell membrane and the cell nucleus. They discovered that terbium-161 bound to a membrane-localising linker peptide, 161Tb-DOTA-LM3, was highly effective at exploiting the short-range Auger electrons of terbium-161. They also, once again, demonstrated the improved efficacy of terbium-161 conjugates versus its lutetium-177 counterparts.
Bringing terbium-161 to the clinic
The success of this work brings fulfilment of the ultimate goal of this work in sight. Van der Meulen's group are currently developing the upscaling of terbium-161 production. In 2022, terbium-161 will be brought to the clinic. An SNSF project, a collaboration between Professor Roger Schibli, head of CRS, and Professor Damian Wild at the Basel University Hospital will perform Phase 0 and Phase 1 clinical trials with membrane localising 161Tb-DOTA-LM3 in humans. To achieve this goal, another collaboration based at the PSI CRS is essential. The production of 161Tb-DOTA-LM3 to required standards for the clinic will be performed by the Clinical Drug Supply group of Susanne Geistlich using the clean room facilities at the CRS, which enable the manufacture of safe radiopharmaceuticals to Good Manufacturing Practice (GMP) standards.
Text: Miriam Arrell / Paul Scherrer Institute
© PSI provides image and/or video material free of charge for media coverage of the content of the above text. Use of this material for other purposes is not permitted. This also includes the transfer of the image and video material into databases as well as sale by third parties.
Contact
Dr. Cristina Müller
Group Leader Nuclide Chemistry
Paul Scherrer Institute
Forschungsstrasse 111
5232 Villigen PSI
Switzerland
Telephone: +41 56 310 44 54
E-Mail: cristina.mueller@psi.ch
Dr. Nick van der Meulen
Group Leader Radionuclide Development
Paul Scherrer Institute
Forschungsstrasse 111
5232 Villigen PSI
Switzerland
Telephone: +41 56 310 50 87
E-Mail: nick.vandermeulen@psi.ch
Original Publications
Terbium-161 for PSMA-targeted radionuclide therapy of prostate cancer
C. Müller , C. A. Umbricht, N. Gracheva, V. J. Tschan, G. Pellegrini, P. Bernhardt, J.R. Zeevaart, U. Köster , R. Schibli , N. P. van der Meulen
Eur J Nucl Med Mol Imaging (2019) 46(9):1919-1930.
DOI: 10.1007/s00259-019-04345-0
Combination of terbium-161 with somatostatin receptor antagonists-a potential paradigm shift for the treatment of neuroendocrine neoplasms
F. Borgna, S. Haller, J.M. Monné Rodriguez, M. Ginj, P.V. Grundler , J. R. Zeevaart , U. Köster , R. Schibli, N.P. van der Meulen, C. Müller
Eur J Nucl Med Mol Imaging (2021)
DOI: 10.1007/s00259-021-05564-0
Further Information
Center for Radiopharmaceutical Sciences (CRS) | CRS | Paul Scherrer Institut (PSI)
Cancer medicine using PSI’s neutron source | Our Research | Paul Scherrer Institut (PSI)
Novel and emerging medical radionuclides | Our Research | Paul Scherrer Institut (PSI)